Robotic Surgery
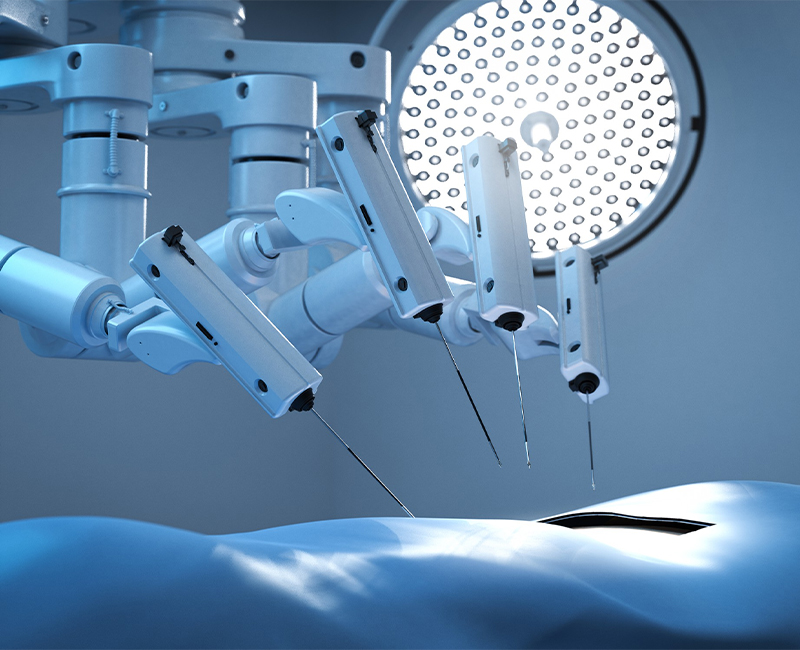
For cancer patients who require surgery as part of their treatment, our doctors sometimes rely on robotic surgery to help remove hard to reach tumours, shorten surgery times or lessen side effects for patients compared to traditional surgery. These tools first made their appearance in the late 1990s and are becoming more and more common in operating rooms. Robotic surgery doesn’t mean that a robot is performing the operation. Instead, it refers to when surgeons direct the surgery using robotic tools. Robotic surgery systems use one or more robotic arms that surgeons control remotely and precisely using a nearby console. Robotic surgery, or robot-assisted surgery, allows doctors to perform many types of complex procedures with more precision, flexibility and control than possible with conventional techniques. Robotic surgery is usually associated with minimally invasive surgery — procedures performed through tiny incisions. It is also, sometimes, used in certain traditional open surgical procedures.
Potential benefits of robotic surgery for patients include
- Reduced pain
- Lower risk of infection or complications
- Less blood loss (fewer transfusions)
- Shorter hospital stays
- Less scarring due to smaller incisions
- Faster return to normal activities (e.g., sexual function, urinary continence)
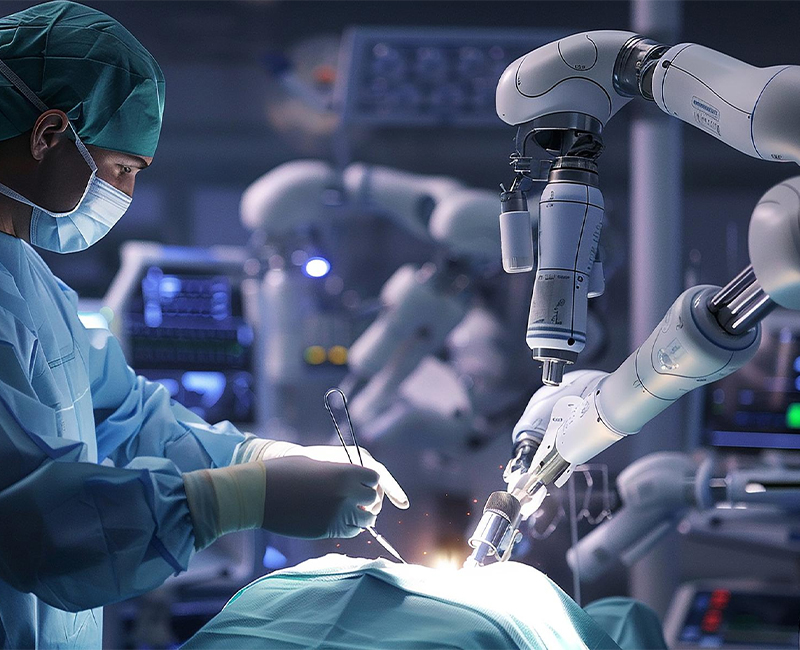
How Robotic Surgery Works
With the da Vinci system’s ergonomic design, the surgeon operates from a comfortable, seated position at a console, with eyes and hands in line with the instruments, and a magnified, high-definition 3-D view of the target anatomy. Some potential advantages of da Vinci Surgery include:
- Greater surgical precision
- Increased range of motion
- Improved dexterity
- Enhanced visualization, including areas that may not be seen by the naked eye
- Improved access to hard-to-reach areas
- Improved ability to spare healthy tissue not impacted by cancer
Frequently asked questions
In the initial few days of an Autologous BMT, the patient will be given booster injections to mobilize stem cells in the blood. Following 4-5 days of booster injections, the patient will undergo a process similar to blood donation called stem cell apheresis. Suppose the dose of stem cells collected is of a sufficient quantity, in that case, the next step will be to give chemotherapy which can last for anywhere between 1-6 days depending on the type of preparative regimen. Following this, the patient will need to be in the BMT unit approximately for the next two weeks, until the recovery of blood counts. Stay in the BMT unit is to monitor the clinical condition of the patient and to ensure that patient is protected from infections.
In this, the type of stem cells used will be the donor stem cells. The patient will initially have to undergo the preparative regimen, which may consist of only chemotherapy or chemotherapy and radiation. Following this, the patient will receive the donor stem cells, which is just like receiving a blood transfusion. Subsequently, the patient will have to stay in the BMT unit for another 2-3 weeks till recovery of blood counts. On average, a patient undergoing Allogenic BMT will have to stay in the hospital for anywhere between 2-3 weeks. During this period, the patient is continuously encouraged to maintain some level of physical activity depending on the functional capacity. The help of the Physiotherapy team is taken to enable this. The patient is supported on a diet which varies depending on the phase of the transplant and dietician’s advice. This food will have to be prepared under strict aseptic precautions and transported from the kitchen to the unit in sealed containers to maintain hygiene. Patients are also encouraged to indulge in various forms of activities like reading, writing, meditation exercises, hobbies like craft-making or playing music to ensure that the mind is relaxed and ready to deal with any stress or anxiety. The patient is usually discharged when the blood counts have sufficiently recovered (a phenomenon called – engraftment) and if there are no signs of graft versus host disease.
Since the patients will be subjected to a high dose of chemotherapy, patients become more susceptible to variations in blood levels with an increased risk of infection and bleeding. There might be inflammation of the gastrointestinal tract leading to pain while swallowing and loose stools. Stomach aches and vomiting are a common feature due to gastric irritation from all the medications. Depending on the type of BMT done, a condition called Graft Versus Host Disease (GVHD) may arise. Some of the rarer side effects include Veno-occlusive disease (VOD), cardiac and renal dysfunction.
In patients undergoing an Allogenic BMT or a Haplo-identical BMT, where the stem cells are from a donor and not-self, there is a chance that the donor immune cells might not recognize the host cells and attack them as foreign cells. This attack can happen either within the first 100 days of the BMT – called Acute GVHD or later up to a couple of years (Chronic GVHD). To reduce the incidence of GVHD, any patient who undergoes an allogeneic BMT or haploidentical BMT will also receive medications to suppress the immunity.
The patient who has undergone an Autologous BMT usually resume full functional activities by 6-8 weeks. The patients who have had an Allogenic BMT, typically need to be monitored regularly for up to 6 months. This monitoring may include hospital visits weekly to check for any signs of GVHD and adjust the dose of immune-suppression medications.
For everyone who undergoes a BMT, it will be a life-changing experience, and with time, patients will adapt to a new normal. Within a few months of completing a BMT, patients will regain most of their functional capacity and will be able to re-integrate back into their regular social life. Some of the long term changes include hormonal imbalances, depending on the age, risk of developing infertility and rarely, reduction in heart or lung capacity.
Patients who are suffering from a variety of cancerous and non-cancerous blood disorders can be offered the option of a bone marrow transplant. The blood cancers in which a BMT has a curative role include:
• Acute Myeloid Leukaemia with High risk and relapsed disease.
• Acute Lymphoblastic Leukaemia with High risk and relapsed disease.
• Multiple Myeloma
• Relapsed Hodgkins Lymphoma
• Relapsed Non – Hodgkins Lymphoma – High grade
• High-risk Chronic Myeloid Leukaemia.
The non-cancerous blood disorders where BMT plays a curative role include:
• Thalassemia Major
• Sickle cell anaemia
• Paroxysmal Nocturnal Hemoglobinuria
• Primary Immunodeficiency disorders
• Aplastic Anaemia.
In particular, solid cancers which generally occur in the younger age group like Neuroblastoma and Ewings Sarcoma, BMT has a role in treatment.
